Friday, July 28, 2006
Thursday, July 27, 2006
Cocky Roach

Patience is the virtue of the least phylogenetically evolved. That is why a creature like this, and its distant unicellular and acellular cousins, will not only inherit the Earth, but also establish thriving communities on Mars, when machines have made us obsolete and we are nothing more than memories in a sepulchered database. Dr. Al

Leave the 2005 Annata in the Wine Cellar
Back to the Horse
Tuesday, July 25, 2006
Monday, July 24, 2006
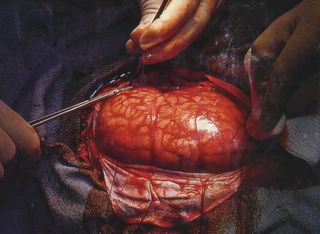
Einstein Autopsy
Sunday, July 23, 2006
Poe-sting
From childhood’s hour I have not been
As others were; I have not seen
As others saw; I could not bring
My passions from a common spring.
From the same source I have not taken
My sorrow; I could not awaken
My heart to joy at the same tone;
And all I loved, I loved alone.
Then in my childhood, in the dawn
Of a most stormy life was drawn
From every depth of good and ill
The mystery which binds me still:
From the torrent, or the fountain,
From the red cliff of the mountain,
From the sun that round me rolled
In its autumn tint of gold,
From the lightning in the sky
As it passed me flying by,
From the thunder and the storm,
And the cloud that took the form
When the rest of Heaven was blue,
Of a demon in my view.
We come into this world alone, and our exit bars variation. Dr. Al
The Perfect Imperfect
With all of its flaws and all of its shortcomings, it is still perfectly imperfect. Furthermore, it's all we've got. So, massage your shiny steel laptops, but cherish and protect the primordial spark resting on your shoulders. We spend much of our lives looking out. Perhaps the time would be better spent looking in. Dr. Al

Saturday, July 22, 2006
Body Traitor
Friday, July 21, 2006
Your ABCDEFs

Your ABCDEFs, in the form of antithrombotics, beta blockers and blood pressure control, cessation of smoking and cholesterol lowering therapy, diabetes management and healthy diet, exercise 3-4 times a week, and fatty fish or fish oils, can quell the raging fires of acute coronary syndrome in that pressure cooker in our chests. Dr. Al

Complicit Corazón
Wednesday, July 19, 2006
Supercalafragilistichemochromatosis
But let’s not put the cart before the horse. Hemochromatosis, like any other hematologic disorder, must be affronted in an orderly, systematic manner. It is currently the most common cause of iron overload in the United States, with as much as 10 percent of the population heterozygous for this condition, and subject to a 25 percent risk of developing minor, apparently harmless increases in body iron stores. For the 0.5 percent of the population homozygous for hemochromatosis, the genetic defect results in an abnormality in the control of iron absorption that causes an inappropriate increase in iron uptake and a progressive buildup of body iron.
And if that were not bad enough . . . . . . ., the iron accumulates as hemosiderin in liver prenchymal cells (hepatocytes), and subsequently in the pancreas, heart, adrenal glands, testes, pituitary gland, and kidneys, leading eventually to hepatic, pancreatic, and cardiac dysfunction and insufficiency and hypogonadism. Women, take heart, however (and please excuse the pun), as the disease usually occurs in males and is rarely recognized before the fifth decade. Ten to twenty years postmenopause is the time-frame for targeted women.
Now, let’s get down to the nitty-gritty, and some of the “gorier” aspects of hemochromatosis. The classic tetrad of clinical signs is hepatomegaly and liver disease, diabetes mellitus, skin pigmentation (combination of slate gray due to iron and brown due to melanin, sometimes resulting in bronze color), and gonadal failure (impotence). Cardiac failure develops in about 10 to 15 percent of untreated patients, with arthropathy and bleeding esophageal varices bringing up the rear. Furthermore, in patients who develop cirrhosis due to hemochromatosis, there is a 15 to 20 percent incidence of hepatocellular carcinoma. So, the picture isn’t pretty!
Body iron stores have usually increased from the normal amount of 1 gram or less to 15 to 20 grams or more by the time symptoms of organ damage appear. Environmental factors, including dietary iron content and alcohol use, as well as the coexistence of other hereditary hematologic disorders, may also greatly influence the rate and severity of organ damage.
So, how do we screen for this polymorphic intruder, who bides its time and lies in wait at our very doorsteps, ready to spring when the genetic equinox is favorable? Screening, after all, is the point of this article.
Needless to say, a high degree of clinical suspicion must be maintained in patients with a family history of hemochromatosis or otherwise unexplained mild liver test abnormalities. For screening purposes, liver function tests (including enzyme assays) and measurements of the plasma iron, transferrin (iron-carrier protein) saturation, and plasma ferritin (storage form of iron) provide the best indirect means of screening. If any of these measurements is abnormal, further evaluation is indicated. Computed tomography (CT) and magnetic resonance imaging (MRI), however, are not sensitive enough for screening asymptomatic persons. Liver biopsy, on the other hand, which characteristically shows extensive iron deposition in hepatocytes and usually in bile ducts, vessel walls, and supporting structures, permits a definitive diagnosis. Further confirmation derives from determination of the hepatic iron index on a liver biopsy specimen (hepatic iron content per gram of liver converted to micromoles and divided by the patient’s age). A hepatic iron index greater than 1.9 suggests hemochromatosis.
However the diagnosis of hemochromatosis is established, screening of family members at risk for the disease is obligatory. Screening should include not only siblings, but also parents and children because of the possibility of homozygous-heterozygous matings.
Which brings us now to the matter of treatment, both in the cirrhotic patient and, more importantly, in the precirrhotic phase of hemochromatosis. Weekly phlebotomies of 500 milliliters of blood (about 250 milligrams of iron), continued for up to 2 to 3 years, achieve depletion of iron stores. When that is achieved, maintenance phlebotomies (every 2 to 4 months) are continued. Now, although the chelating (binding) agent, deferoxamine, administered intramuscularly, has been shown to produce urinary excretion of 5 to 18 grams of iron per year (comparing favorably with the rate of 10 to 20 grams of iron removed annually by weekly or biweekly phlebotomies), the treatment is painful and requires a constant infusion pump. Furthermore, active treatment of the complications of hemochromatosis - arthropathy, diabetes mellitus, heart disease, portal hypertension, and hypopituitarism - may be necessary. A multifaceted approach is the name of the game.
So, what is the “silver lining,” if, indeed, there is one? In precirrhotic patients, phlebotomy therapy can prevent the onset of cirrhosis, while at the same time reducing cardiac conduction defects and lowering insulin requirements. In patients with cirrhosis, bleeding esophageal varices may be reversed, but, unfortunately, the risk of hepatocellular carcinoma still lurks in the shadows.Vigilance and aggressive therapy are the only options available to turn down the volume on our “Supercalafragilistic-hemochromatosis.”
Tuesday, July 18, 2006
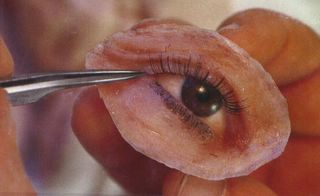
Eye-atollah
Simply put, a cataract is nothing more than a painless, cloudy area in the lens of the eye, which blocks the passage of light from the lens to the nerve layer of the retina. Unlike a sultan’s harem, which at the least has vigilant, muscularly well-endowed eunuchs to halt the march of an unholy infidel, the retina is defenseless to the onslaught. In fact, some cataracts grow larger or denser over time, causing severe vision changes leading to blindness, glaucoma, or a loss of independence in older adults.
While aging, ultraviolet radiation from sunlight, eye injury, poorly controlled diabetes mellitus, glaucoma, steroid medications, and frequent radiation treatments of the head all contribute to the clouding effect of cataracts, some degree of lens opacity is expected in everyone over the age of 70.
Risk factors for cataracts are as multivariegated as the colors of a Persian rug, and some of them can literally represent straws to break a camel’s back. There are those, for example, that one cannot change, such as age 65-74, Native American and African American race, female sex, and family history. Others, like life-long, chronic diseases (diabetes, glaucoma, and high blood pressure), when kept in check, can be temporarily thwarted in the inexorable march toward cataract. Still other risk factors, for example chickenpox during pregnancy, smoking, exposure to ultraviolet light, long-term use of steroid medications, and even alcohol, should not be underestimated.
So, when does cataract warrant the same concern demonstrated by the head of a clan, unable to find a suitable husband for the eldest of his eight daughters? Severe eye pain, sudden change in vision or eyeglass prescription, and blurred or double vision all mandate recourse to the healing arts. Surgery becomes necessary when vision loss caused by a cataract affects the patient’s quality of life. Until then, not smoking, wearing sunglasses in the sun, eating a diet rich in vitamins C and E, limiting alcohol intake, avoiding steroid medications, keeping high blood pressure and diabetes under control, taking estrogen for menopause, and using mydriatic eyedrops to dilate the pupil do as much to prevent or postpone surgery, as a “toke” on a water pipe and a good cup of Turkish coffee do to make a reluctant suitor more malleable to the manipulative whims of a prospective father-in-law.
When standard extracapsular surgery, in which the lens and its anterior membrane are removed, or extracapsular surgery using phacoemulsification, in which sound waves are used to break the lens up into small pieces, becomes necessary, subsequent placement in the eye of a new intraocular lens will usually guarantee most adults 20/40 vision or better within 3 weeks to 2 months after surgery.
It therefore goes without saying that, dollar for dollar, an ounce of prevention and informed consent do far more than smart bombs and cruise missiles to halt unwanted incursions of the “Eye-atollah.” Remember, cataracts are no fun, and belly dances are performed at night!
Copyright 2003, Albert M. Balesh, M.D. All rights reserved.
Elder-bury Whine
Over the next 3 decades, the number of individuals over 65 years old will almost double, going from 29 million to over 51 million in the year 2020. This group will represent 17% of the total population. Currently, over 21% of all first admissions to state and county mental health facilities in the U.S. are over 65 years old. Furthermore, depression is particularly prominent in the geriatric population, with those over 65 committing suicide at a rate higher than any other group in the U.S.
Medicine cabinets crammed full of a vast assortment of multicolored elixirs and “bonbons,” upon which we rest our hopes for the future, are the envy of every “kid in the candy store.” Exercise and healthy diet, too, have ceded the sidewalk to “pushers” in three-piece suits, who hawk their wares to the tune of billions of dollars in annual pharmaceutical revenues. Ninety-five percent of people over 65 now take some type of medication.
As we get older, we see a decrease in gastric-cell activity, resulting in a rise in the gastric pH. Blood flow to our abdominal viscera decreases, intestinal motility declines, active transport processes are altered, and slight of hand produces no rabbit, but rather laxative or Milk of Magnesia.
There is a decrease in total body water with aging, as well as a reduction in lean body mass. Body fat increases, and the increase in adiposity with aging results in a greater amount of drug stored in the periphery of our bodies. This in turn prolongs the time required to metabolize those drugs. Serum albumin levels also decrease 15 to 20% with age, and the concentration of free drugs (not bound to albumin, and therefore free to act) subsequently increases. That increase gives rise to more side effects, since more drug is now available to enter tissues.
Many drugs are metabolized in the liver to active and inactive metabolites. Still, in those 65 years old and older, hepatic blood flow is decreased by 40% as compared to a young adult. This results in both a great degree of individual variation in liver metabolic activity in the aged and toxic buildup.
When we were young, a right of passage was not “peach-fuzz” as a preliminary to beard stubble, but rather the distance and sheer power of a urine stream. However, when our “plumbing” ain’t what it used to be, the processing of our bodies’ toxic waste tends to decrease. In fact, the rate at which we process a given quantity of toxic waste decreases 50% by age 70. A decrease in renal blood flow with age adds to the picture.
Perhaps it is just plain better to die young. A diet rich in vitamins and antioxidants, combined with stimulating play, nonetheless, can slow or reverse some age-related brain deterioration in dogs, which are a good model of human aging.
An occasional glass of elderberry wine, too, helps “bury” the elderly whine . . . . .
Copyright 2003, Albert M. Balesh, M.D. All rights reserved.
Staying Abreast
While two thirds of the tumors in reproductive age women are benign, the majority of lesions in postmenopausal women are malignant. Routine monthly self-examination and yearly physician evaluation are recommended for all women over age 20. Self-examination should be performed approximately 5 days after menses, when the breast is least engorged and tender.
One in every 9 American women will develop breast cancer during her lifetime and will have a 3.5% chance of dying from it. The risk of contracting it increases with age. Yet, while the incidence of diagnosis is increasing, the death rate is decreasing, most likely due to earlier detection and improved therapies.
Although “girls just wanna have fun,” they must be made aware of the fact that abstinence from alcohol and a low-fat diet are integral to the prevention of breast cancer. Women who live in warmer climates have a lower risk (1.5 times) for breast cancer than those living in cold, northern regions. Significant risk factors for breast cancer include increasing age, a family history of gynecologic malignancies, a first-degree relative with breast cancer, exposure to ionizing radiation before age 30, and significant alcohol use.
Some physicians suggest that estrogen replacement given with progesterone may actually decrease a woman’s risk of breast cancer, just as it does the risk of endometrial cancer. Others categorically disagree with that opinion.
Breast cancer patients present clinically with masses, skin change, nipple discharge, or symptoms of metastatic disease. Palpable masses are most often detected by the patient on self-examination and are usually nontender, irregular, firm, and immobile. Fifty percent of tumors occur in the upper outer quadrant of the breast.
Mammography is the best tool to detect early lesions, reducing mortality by 30-50%. The American Cancer Society currently recommends a baseline screening mammogram at age 35-39, a mammogram every 1-2 years between the ages 40-50, and a mammogram annually after age 50. Patients who present with weight loss, anorexia, fatigue, shortness of breath, cough, and pain should set off “buzzers” and “flashing lights.”
Wide local excision, lumpectomy, and segmental mastectomy are breast-conserving treatments. Candidates are eligible for them if the tumor is 4 cm or smaller, with no fixation of the tumor to the underlying muscle or to the chest wall, no involvement of overlying skin, and no multicentric lesions or fixed lymph nodes. Depending on tumor stage, the 5-year disease-free survival rate in patients with breast cancer varies. The current overall 5-year survival rate has now increased to 94%.
As a physician, my “staying abreast” and your “staying abreast” of the issue is tantamount to “staying alive.”
Copyright 2003, Albert M. Balesh, M.D. All rights reserved.
Saturday, July 15, 2006
Mr. Trouble: Daily Dilemma of Diabetic Decay
First things first. Time for a “pit stop.” It seems like I live in the bathroom. I urinate a lot, and thirst is a constant companion, too. I’m always reaching for that “mythical nectar,” which will finally calm the fires raging in my mouth and tame my insatiable hunger. They say that breakfast is the most important meal of the day, and I often eat it like there’s no tomorrow. Then the praying begins. I try to relieve myself with the day’s “number two” before I leave for work. My bowel is lazy, however, and the color, smell, and sheer number of Trojans extruded from this horse are enough to make a man sick. My digestive powers are basically defunct.
My eyes aren’t what they used to be either. My doctor says that the hemorrhages inherent in my malady have taken their toll on my retina. I don’t see as well as I used to, and images are a constant blur. The trip to work scares me to death, and my car bears the scars of my visual shortcomings.
No sooner do I arrive on the job than my energy level suddenly falls. Fatigue is my guardian angel who I cannot give the slip to. Irritability is my middle name, and all it takes is a kind word to set me off. My fast and shallow breathing, as well as the strong, fruity nature of my breath, betray vice more than illness. My boss’s eyes don’t lie, and my coworkers politely distance themselves from me. They know that I have been losing weight, and they halfheartedly offer to take me out to lunch. I can’t accept, however. I must find some nook, cranny, or cubbyhole in which I can gain an hour’s respite from mitochondrial drain.
I’m what you call a compliant patient. I try to watch my diet, perform regular, daily testing of my blood sugar level, and take my medications religiously. I know that by following this procedure and my doctor’s advice, I can slow the onslaught of what may be the inevitable. Perhaps it is already too late.
Day is done, and I cross the threshold of my abode, so tired that I can barely lift my head. I live alone, a leper, afraid to subject healthy females of the species to my shame, my guilt, and my nightmare. Even if I could pick up the phone and call one of my old flames, the numbness of my flesh could never translate into a “healthy tingling.”
But what have I done? Why am I being tortured? Why doesn’t God punish charlatans, ambulance chasers, politicians, college administrators, Enron executives, and Martha Stewart instead? Why me? I guess it’s because “Mr. Trouble” is my name, and I must bear the weight of the “scarlet D” on my tunic.
Motor Madness
Motor-vehicle crashes are the leading cause of death in the United States for persons ages 1-34, according to the National Center for Health Statistics. Thirty-eight percent (15,794) of U.S. traffic fatalities in 1999 were alcohol-related; on average, drinking and driving killed a human being every 31 minutes. Furthermore, about 3 in every 10 Americans will be involved in an alcohol-related crash at some time in their lives. If that were not enough, from 1995 to 1996, alcohol-related traffic fatalities among youths ages 15-20 increased by nearly 10%, from 1,473 to 1,617.
We all know that mixing alcohol and other drugs with driving leads to potentially fatal impairment. Like a concoction of oil and water, or the mating of a supermodel with a nerd, they simply don’t mix. It doesn’t take a brain surgeon to know that blood alcohol concentration (BAC), expressed as the percentage of alcohol in deciliters of blood - for example, 0.10% is equal to 0.10 grams per deciliter, correlates with the risk of fatal traffic accidents. Compared with drivers who have not consumed alcohol, the risk of a single-vehicle fatal crash for drivers with BACs between 0.02% and 0.04% is estimated to be 1.4 times higher; for those with BACs between 0.05% and 0.09%, 11.1 times higher; for drivers with BACs between 0.10% and 0.14%, 48 times higher; and, finally, for those with BACs at or above 0.15%, the risk is estimated to be 380 times higher.
What can we do? Who can we turn to for help? After all, even our ministers and priests have been known to take an occasional “snort” or two. Our therapeutic thrust must follow seven lines of reasoning. First, we must examine risk factors such as personality, social environment, anxiety, depression, loneliness, genetics, and type of drug. Second, family, friends, or co-workers must take an active role in persuading a loved one to undergo screening for drug addiction. Third, family physicians must be reminded that a diagnosis of drug addiction often starts with them. Fourth, we must be aware of the disruptions wreaked on our family, work, social, school, legal, and financial lives by dependence on drugs. Fifth, the expedience of detoxification on an outpatient basis must be contemplated. Next, parents must be educated to communicate, listen, set a good example, and establish a strong, stable bond with their children. And, finally, counseling services, treatment programs, and self-help groups must be sought out after detoxification has run its course.
“Wired, tired and perspired” is neither safe nor acceptable behavior when driving a motor vehicle or checking-in at an airport.
Copyright 2003, Albert M. Balesh, M.D. All rights reserved.
Cupid's Conceit
At the top of our list is the subject of depression, which can be triggered by the onset of heart disease. That finding may, indeed, account for the increase in depression afflicting those of us 45 years of age and older. High cholesterol and coronary artery disease have been linked to inflammation of the immune system, which, in turn, is related to the neurotransmitter serotonin. As brain serotonin levels are known to affect mood, it takes no stretch of imagination to deduce the logical connection between a sick heart and a sick mind.
The connection between heart disease and depression has led to new strategies to reverse the latter. Lowering cholesterol and losing weight may have a distinct impact on depression. Furthermore, supplements that contain natural anti-inflammatories - such as omega-3 fatty acids - may also help to stop the cascade of chemical events associated with the symptoms of a wounded psyche.
Let us now turn our attention to “Fat America,” and the 36 million of us who need drugs to control our cholesterol levels. Target cholesterol levels depend on age (men 45+, women 55+), sex and family history, and risk factors, such as smoking, abdominal obesity, high blood pressure, high blood sugar, low HDL (“good” cholesterol), diabetes, and high triglycerides. It is all a simple matter of numbers. A person with only one heart-attack risk factor can live comfortably with an LDL (“bad” cholesterol) score of 160 (in milligrams per deciliter of blood). Those of us with two or more risk factors require a lower LDL level (130), and those already suffering from diabetes or heart disease even lower (100).
While drugs like Mevacor and Pravachol have few side effects and undeniably prevent heart attacks by lowering LDL, one has to question the wisdom and economics of creating 36 million “junkies” with $800-a-year drug-regimen habits. Certainly, an even simpler measure is preferable. Eating six small meals a day, instead of the usual two or three large ones, can, indeed, lower cholesterol count.
Finally, a study published last year in the January 9, 2003 issue of The New England Journal of Medicine determined that regular, moderate consumption of alcohol may lower men’s risk of heart attacks. Unfortunately, although women may receive some of those benefits, the risk of dying of breast cancer is 30 percent higher among those who drink alcohol at least once a day.
When the acne-spotted youth finally comes of age, there will be much more to worry about than an arrow through the heart or a missed valentine. Cupid will move on to other quarry, but, in our conceit and overindulgence, we may be left with the wounds of darts from a far more imperious quiver.
Copyright 2004, Albert M. Balesh, M.D. All rights reserved.
Thursday, July 13, 2006
Vege-toll
Do we heat our vegetables or eat them raw? Nutritionists agree that eating fruits and vegetables raw is a healthy way to get water, fiber, and vitamins. Nonetheless, that should not be a blanket statement, as there are others who are convinced that some foods are healthier cooked. Cases in point are the examples that follow.
Most fruits, as well as spinach, broccoli, cabbage, cauliflower, and red and green peppers, are healthier when eaten raw. In general, they are essentially quite high in vitamins B, C, folate, and potassium when eaten uncooked. Strawberries are especially nutritious and contain the cancer-fighting phytochemical called ellagic acid, which may be diminished or destroyed by cooking. Uncooked red and green peppers contain numerous antioxidants called polyphenals. The old adage, “Everything in moderation,” must not be overlooked, however, as too much spinach, broccoli, cabbage, and cauliflower can cause indigestion and the unleashing of an individual chemical attack that would make even Saddam Hussein blush.
Tomatoes, carrots, lima beans, black-eyed peas, navy beans, soy beans, sprouts (alfalfa, clover, etc.), potatoes, and corn live on “the other side of the tracks.” It is smarter to cook them. Tomato sauce, paste, and ketchup have higher levels of leucopene, an antioxidant that protects against cancer and heart disease, than raw tomatoes. Leucopene is easier to absorb after a tomato is cooked, but cooking destroys some of the vitamin C in tomatoes.
Blanching (quickly boiling) and pureeing carrots increases levels of antioxidants by 34 percent, and allows the body to absorb more beta-carotene. Illegitimate children of the Bean Family (lima beans, black-eyed peas, navy beans, and soy beans) can attain a degree of respectability and a birthright through higher temperatures. Eating those legumes raw not only hinders the absorption of certain nutrients, but can irritate the gastrointestinal tract as well. Starchy vegetables are indigestible when raw, causing gas and indigestion.
Sprouts like alfalfa and clover can carry salmonella and E. coli bacteria when raw, and cooking them is strongly advised.
So, while “an apple a day keeps the doctor away,” unexpected detours to the oncologist can be avoided by paying one’s “vege-tolls” on the road less traveled.
Copyright 2004, Albert M. Balesh, M.D. All rights reserved.
The Al and Joe Medicine Show
From north to south and east to west, in circus sideshows, medical literature, and the hallowed halls of prestigious research institutions, hawking medicinal wares has become a quotidian way of life. “Take this pill for gas, that one to make a baby, and a drop of Kaopectate to prevent those nasty squirts.” Damn the long clinical trials, turning back the hands of time has become big business. In an epoch where the good die young and the old die miserably, edges and hedged bets are desperately sought.
March 2004, as National Nutrition Month, beckons us all, as captains of our protoplasmic ships, to throw Al and Joe overboard and set a course that will take us the long way around. Living longer, more productive lives, with an emphasis on quality of life, and freeing children from the ethical and financial handcuffs of caring for aging, “baby-boomer” parents in frail health is our destination.
It has been shown on numerous occasions that the risks of type 2 diabetes mellitus and stroke can each be lowered by 30 percent with brisk walking two to three hours a week. High blood pressure can also be reduced or prevented with moderate exercise, and osteoporosis and bone fractures will occur less often. Furthermore, three hours of brisk walking a week will lower the risk of heart disease by 40 percent.
Those pesky little vitamins that we sometimes think are so good must be carefully scrutinized for benefits, side effects, and cause and effect. Very large amounts of vitamin A can harm bones, make hip fractures more likely, and cause brain damage, liver damage, and birth defects. Folic acid can increase the risk of neurological problems in people lacking adequate vitamin B12, and the anemia caused by high doses of vitamin C is no laughing matter. High doses of vitamin D can cause dangerously abnormal blood levels of several minerals. Finally, vitamin E can cause excessive bleeding in surgical patients or people taking anticoagulants such as warfarin.
French researchers have found that people who eat fish at least once a week are less likely to develop dementia. It has been suggested that fish oils (particularly omega-3 fatty acids) are at the heart of the matter, and help control inflammatory processes that are associated with Alzheimer’s disease. Don’t forget to take French wine “to heart” also.
The high-fat, low-carbohydrate diet, first introduced back in 1972, is based on the premise that heavy carbohydrate consumption causes the body to store more food as fat, and reducing the intake of carbohydrates subsequently forces fat reserves to be burned. Balanced nutrient diets (1984), which limit daily intake to 30% protein, 30% fat, and 40% carbohydrate, stimulate the body’s ideal production of the hormone insulin, which in turn encourages weight loss. Back-to-basics diets (1988), which cut out grains like white flour, promote consumption of fruits and vegetables, and substitute free-range animal meat for fatty, grain-fed beef, herald a return to the nutritional habits of our ancestors. Finally, the high-fiber diet (1990) favors consumption of vegetables, beans, whole grains, and fruit, as well as low-fat dairy products like skim milk, nonfat yogurt, and egg whites in moderation. Meats, oils, olives and sugar are avoided as much as possible.
“Sell it, Joe. Sell it all! Maybe we can earn enough Frequent Flyer miles to blow this place for good.”
Copyright 2004, Albert M. Balesh, M.D. All rights reserved.
Forty Winks or Forty Wives?
I was like the 70 million other problem sleepers in this country. I just couldn’t get my act together. I might as well have climbed Mount Everest or won the Texas Lottery. My complaints were not singular either. They ran the gamut from restless legs syndrome, advanced sleep phase syndrome (ASPS), and delayed sleep phase syndrome (DSPS) to even sleep apnea.
Pain, stress, stimulant medications, anxiety, regular use of over-the-counter sleeping pills, depression, alcohol, lack of physical activity, poor sleep habits, and changes in my lifestyle and environment had all conspired against me. All I needed was forty good winks, and yet, every night I was besieged by forty bad wives.
To make matters worse, those voices in my head were exacting a toll on my performance the next day. Now, granted, I knew that the average American now sleeps about seven hours a night, about 90 minutes less than people did a century ago, but my conundrum took this to the nth degree. The convincing evidence I read that untreated sleep disorders can increase the risk of high blood pressure, coronary-artery disease, heart failure, and stroke was like a cold shower.
I also started to notice a potbelly, and getting into my pants became comparable to wearing an athletic supporter. Then I read that lack of sleep can increase the odds of developing obesity and diabetes. That was the final straw! I learned that there are five stages of sleep, and that my problems most likely stemmed not from the light sleep, transition, or deep sleep stages, but rather from the REM sleep stage (where vivid dreams appear). And my dreams were becoming “vivid,” to say the least, as one of my wives, “Wanda,” was now beginning to take on the physiognomy of a “Juan.”
I decided to consult the “Three Kings:” my mother, my naturopath, and my druggist. Warm milk, turkey, and tennis balls were my mother’s remedies for what ailed me. Warm milk (containing a precursor of melatonin), turkey (filled with sleep-inducing tryptophan), and tennis balls (sewn to the back of my T shirt to prevent snoring by keeping me on my sides) bordered on the ludicrous.
My naturopath suggested valerian, aromatherapy with chamomile and lavender, melatonin (which added to my nightmares and increased the wife-count to sixty), and hops (which padded my already-high Budweiser bill) for the modest, all-inclusive price of $250.
My druggist, on the other hand, was the most sympathetic of all. He recommended the non-addictive Sleep-Eze, Sominex, and Dormin (over-the-counter antihistamines), as well as Halcion (quick-acting but addictive) and Sonata (a romantic name for a short-acting, non-addictive sleep aid). He even suggested a prescription antidepressant called Desyrel, but warned me that it might cause painful erections.
In the end, rather than pursuing the quest ad infinitum, I decided to take control and follow my version of the Ten Commandments: 1) sleep only when drowsy; 2) maintain a regular rise time; 3) use the bedroom only for sleep and sex; 4) avoid napping during the daytime; 5) avoid caffeine within four to six hours of bedtime; 6) avoid the use of nicotine close to bedtime; 7) ban alcohol within four to six hours of bedtime; 8) avoid large meals before bedtime; 9) avoid strenuous exercise within six hours of bedtime; and 10) minimize light, noise, and extremes of temperature in the bedroom.
Alas, however, I am a sinner. Commandments were not enough. What I needed was an exorcism. So, I went to the American Academy of Sleep Medicine at www.aasmnet.org, and, I must say, although demons continue to inhabit my inner sanctum, I have begun to file for multiple divorces.
Copyright 2004, Albert M. Balesh, M.D. All rights reserved.
Tuesday, July 11, 2006
Medical Technology: Midas Touch or Dr. Frankenstein?
Copyright 2004, Albert M. Balesh, M.D. All rights reserved.
Stem Cells: You Can't Live with 'Em, You Can't Live without 'Em!
Mine is Bigger than Yours! The Truth about Fertility
Copyright 2004, Albert M. Balesh, M.D. All rights reserved.
Monday, July 10, 2006
TB or not To Be
As you know, tuberculosis is a disease that, because of its airborne transmission, has great public health significance, sometimes pitting the concerns and desires of the diseased individual against the public good. The goals of public health are threefold and include prompt diagnosis and treatment, prevention of transmission to others in the community, and identification of those infected with Mycobacterium tuberculosis who are at high risk for developing disease, and therefore candidates for preventive treatment.
Disease surveillance is of paramount importance. Suspected and confirmed cases of TB must be reported to public health authorities. Following closely on its heels is case containment. By assuring appropriate and complete treatment of cases, the chain of transmission is cut.
There is a saying that “treatment is prevention,” and this should remain the cornerstone of tuberculosis control efforts. The next important task is to target tuberculosis-infected individuals at high risk of developing active tuberculosis, and provide them with preventive treatment. Preventive activities, as you can well imagine, can be quite difficult since the “patient” is not sick. Issues such as adherence to treatment become magnified, and there is absolutely no mandate (and perhaps there should not be one) to require treatment.
Clear national guidelines describing the goals and objectives of tuberculosis control have been published by the Centers for Disease Control and Prevention. It is the responsibility of El Paso’s tuberculosis control programs to implement them.
Tuberculosis has retreated into selected and epidemiologically defined high risk groups, and this has made it harder to attend to public health concerns. Advocacy for tuberculosis control efforts is difficult because those with the disease are seen as “others” who have no relationship or relevance to the public at large, except as threats (for example, foreign born, injection drug users, homosexuals, alcoholics, prisoners, etc.).
The public health sector indeed has some unique responsibilities in terms of tuberculosis control in the El Paso Community. It should provide coordination, management, and oversight of all aspects of tuberculosis control. This sine qua non of public health will ensure that “TB is not To Be.”
Copyright 2004, Albert M. Balesh, M.D. All rights reserved.
Physician Roulette: Come on like Thunder to Prevent Medical Blunder
With 196,000 people dying each year in hospitals from medical errors, careful scrutiny of the diplomas on a wall is just a first step. Common medical errors run the gamut from adverse drug reactions and dispensing blunders, to dirty hands, medical equipment, and catheters, serving as foci of infection. And let’s not forget wrong-site surgery either.
The statistics are absolutely mind-boggling. According to the Food and Drug Administration (FDA), the University of Michigan School of Medicine, the Joint Commission on Accreditation of Healthcare Organizations (J.C.A.H.C.), and the Institute of Medicine: 1) each year 1.3 million people are injured by medication errors ranging from adverse drug reactions to dispensing blunders, and at least 7,000 patients die; 2) 200,000 people are infected by intravascular catheters each year, nearly the same number suffer urinary tract infections from urinary catheters, and, to make matters worse, doctors are unaware that a urinary catheter is in place 40% of the time; 3) two million people each year come down with hospital-acquired infections; and 4) since 1996, there have been 150 reports of surgeries being performed on the wrong limb or organ.
So, what can we, the general public, do to prevent our becoming casualties of this war or, at the least, statistics in some remote medical journal? There are precautions we can take to help prevent some of the more common medical problems, and I will list them here.
1) Monitor your own care.
2) Quiz doctors and nurses closely, even in high-pressure situations like the operating room.
3) Clarify physician handwriting, dosage, and indications for all prescriptions. In other words, read the prescription back to your doctor and ask what it’s for.
4) During a hospital stay, ask every nurse or aide the name of the medicine he or she is giving you, and what it’s for.
5) Be particularly careful and vigilant about medicines with similar names.
6) Provide your physician with a list of all the medications you are currently taking, in order to avoid prescription of a new medication that will interact adversely with another you’re already on.
7) Ask everyone who might touch you to wash his or her hands, to avoid transmission of infection via hospital workers’ hands.
8) Ask your doctor if it’s absolutely necessary to insert a urinary catheter. If the answer is yes, ask when it can be taken out. Also, ask for an antiseptic-coated catheter, and, if insertion is protracted beyond two days, make sure the catheter is made of silver alloy.
9) Make sure you and your surgeon are on the same wavelength. Discuss what steps are being taken to identify the right site for the procedure. Once you’re in the operating room, confirm that everyone on the surgical team knows what procedure has been scheduled and the right site for the procedure.
Rules, guidelines, directives, and shopping lists, like those listed above, are difficult to adhere to in the real world. That’s why the Senate recently passed legislation that would create a voluntary and confidential reporting system for medical errors. Healthy vigilance during clear sailing will help us circumnavigate our years, mindful of, but not intimidated by, possible medical storm clouds ahead.
Copyright 2004, Albert M. Balesh, M.D. All rights reserved.
Bugged!
Historical perspective on the “measles experience” in the United States from 1912 to 1963 gives us a point of departure. The incidence of measles during that period never dropped below 100,000 cases per year, and epidemics were quite common. After the introduction of the first vaccine in 1963, the number of cases fell to very low levels. We are now faced, however, with an entirely new scenario that risks taking us back to square one.
Obtaining pathogens, culturing them in vast quantities, and “weaponizing” them, or turning them into a form that remains virulent, has not appeared to pose a problem to those who seek to undermine our democracy. Anthrax is a relatively common veterinary disease. Collect a little blood from a cow that has died of anthrax (or even get spores from the soil or a carcass), put it in a petri dish, and, “abracadabra,” you have anthrax.
To date, more than 70 bacteria, viruses, parasites, and fungi are serious human pathogens. The anthrax bacillus, for example, can infect skin (20% fatal), lungs (90% fatal), or gastrointestinal (GI) tract (25% to 60% fatal). Anthrax spores can enter the skin through minor cuts, and then grow into toxin-producing bacteria. Skin rash follows, with toxins striking surrounding tissue and immune cells carrying microbes from the skin to the lymph nodes and the rest of the body. Exposure to airborne spores, on the other hand, can result in their deposit in the alveoli of the lungs. After germination of those spores, which in some cases may take up to 60 days, flulike symptoms begin, followed by bacterial multiplication, toxin release, and further deterioration of lung tissue. Immune cells, the “taxicabs” of the body, then ferry the microbes from the lungs to lymph nodes and other sites in the body.
What can we do to prevent this public health nightmare? If you think you’ve been exposed to anthrax, telephone your doctor or your local health department, who will set up immediate lab testing which can quickly diagnose anthrax in blood or nasal secretions. Should you test positive for anthrax, immediate drug therapy will, and should be, initiated.
All forms of anthrax are highly treatable if detected within the first few days of exposure. Drugs are useless, however, once a person develops symptoms. Ciprofloxacin (Cipro), a potent, broad-spectrum antibiotic, is currently being used to treat suspected cases of inhaled anthrax. It should be pointed out, however, that the vast majority of anthrax infections can also be managed with penicillin or tetracycline (Doxycycline). The standard course of treatment is 60 days, or 30 days of antibiotic and a series of three vaccine shots. A preventive vaccine is available to military personnel and scientists, but has not been approved for general use or tested in the general public at large.
There are downsides, however. Ciprofloxacin should not be prescribed to pregnant women or to anyone under 18 years of age, except in known cases of anthrax exposure.
Although clearer heads, comfort levels, government reassurance, and enactment of adequate public health measures will go a long way to curtail panic, we must resign ourselves to the fact that anthrax and other “little fellas” will be around to “bug” us for quite some time. After all, they were here first. Cool heads and rational use of the medical weapons at our disposal, however, will ensure that we are the only ones left standing.
Copyright 2004, Albert M. Balesh, M.D. All rights reserved.
Sunday, July 09, 2006
Flat Tired
Although its cause remains a mystery, like a sudden pneumatic blowout, its effects are evident. One’s normal activities begin to stagnate, and good sleep, whatever that is, simply is no match for the strong and noticeable fatigue that takes over our daily existence. Pedal to the metal, in the form of caffeine and psychostimulants, is no match for the sputter of depressed physiologic machines of all ages and social and economic classes. Women are diagnosed with the malady two to four times more often, and Shakespeare’s “rose” or chronic fatigue syndrome would smell as sweet, whether it be called myalgic encephalomyelitis, postviral fatigue syndrome, or chronic fatigue and immune dysfunction syndrome.
CFS is a chameleon and a great imitator rolled into one. It can begin after a minor illness, such as a cold, or during a period of excessive stress. Finding its cause is infinitely more difficult than pinpointing that obnoxious rattle and hum of a recently purchased used car. Diagnosis is difficult because its symptoms mimic those of other more common diseases, such as influenza. Headache, tender lymph nodes, fatigue and weakness, muscle and joint aches, and inability to concentrate are all part and parcel of CFS, and yet they are nonspecific. Unlike influenza symptoms, however, which disappear in a few days or weeks, CSF symptoms taunt us, demoralize us, and then retreat, only to reappear, like a red dashboard light, when our rpm’s increase.
If that were not enough, not all members of the medical community have embraced the idea of a syndrome that cannot be better defined by specific clinical sign or laboratory test. Furthermore, many patients with CFS also have major psychiatric illnesses, such as depression, which of themselves, and also by virtue of the medicines used to treat them, can cause some of the CFS symptoms. This has led sympathetic clinicians to consider CFS as part of a range of illnesses that have fatigue as a major symptom, and to formalize its diagnosis specifically, only when four of the seven possible symptoms mentioned previously are present and the other causes of the same symptoms have been ruled out.
So, where does that leave us? Do we trade in our old vehicles, or do we still have a few good years left in them? A good doctor, like a good mechanic, must first make an accurate diagnosis before that decision can be made. Diseases that have similar symptoms to CFS must be ruled out. Only then can measures be taken to jumpstart physiology and recharge our proverbial batteries. When a battery cable will just not do the trick, a highly nutritious diet, stress control, a monitored exercise regimen, frequent rest breaks throughout the day, and judicious use of sleeping pills, antidepressants, and analgesics can go a long way to resurrecting fallen soles.
Copyright 2004, Albert M. Balesh, M.D. All rights reserved.
Vaccimum
Certainly, the fact that 56 million Americans, not to mention our legions of friends north and south of the borders, are prey to influenza each year. That, in itself, would not be alarming, if “Jewish penicillin” (chicken soup), comfortable pajamas, a soft, warm blanket, and a few days’ bed rest fueled rapid recovery of our physiologic machines. What grinds the cogs to a halt is the realization that influenza is responsible for 200,000 hospitalizations and 36,000 deaths in the U.S. each year. And that is in no way comparable to tax credits for the rich and privileged, but rather something far more serious: a potential bombshell in the laps of the poor, the sick, the elderly, and the cancer-ridden, those most likely to reap the catastrophic harvest of a flu epidemic.
Up until now, the U.S. had been guaranteed 100,000,000 doses of flu vaccine each year, more than enough to ensure holiday cheer and smooth pursuance of Christmas shopping. Shutdown, however, of a vaccine production plant in Liverpool, England, operated by a U.S. company called Chiron (based in San Francisco), resulted in a 50% shortage of flu vaccine and prospective lumps of coal in fireplace-hung stockings this season, to the chagrin of store merchants and an economy already strapped to its limits.
Without “vaccimum” protection, what can Americans look forward to? Well, a myriad of things come to mind that run the gamut from discomforting but self-limited common colds to life-threatening pneumonias. And that’s not all! Nasal channels, sinuses, eustachian tubes, tonsils, and bronchioles are all affected by the flu, and infection produces mucosal redness and swelling, as well as an overproduction of mucus and symptoms that everyone is familiar with. Also, let us not forget that the influenza viruses mutate to protect themselves from our bodies’ defenses, and that the pandemic of influenza in 1918 killed 20 million people and was caused by a swine influenza virus. That raises the conundrum of animals as “our best friends.”
With current supplies of vaccine limited, certain groups of individuals have been asked to forgo or defer vaccination, and that includes some for whom vaccination was recommended in 2003, such as healthy adults 50 to 64 years of age and household contacts of high-risk persons other than children younger than 6 months of age. On the other hand, the priority groups for vaccination fall into seven categories: all children 6 to 23 months of age, adults 65 years of age or older, persons 2 to 64 years of age with chronic medical conditions, all women who will be pregnant during the influenza season, residents of nursing homes and long-term care facilities, health care workers involved in direct patient care, and out-of-home caregivers and household contacts of children younger than 6 months of age.
As holiday credit card bills mount and children moan for the latest high-priced, technological toys they see on our big-screen, plasma TVs, which we don’t have to pay for, until 2006, we must ask if there is a “silver lining” to nasal passages ripe for phlegm and obstruction. Of course, there is. We can take “vaccimum” solace in the fact that simple precautions, like washing hands, covering mouths, and staying home from work when sick, can slow transmission of influenza. Furthermore, drugs like Tamiflu can make the flu more bearable, in the face of scalpers peddling doses of vaccine at 10 times the normal price and the cost of this year’s flu epidemic hitting $20 billion in medical payments and lost workdays.
What? You say you want to live forever. Maybe I’ll just stay home, bar the windows, and cozy up to my big flat-screen. That won’t do much for my finances, but it may prevent “vaccimal” sniffles.
Copyright 2004, Albert M. Balesh, M.D. All rights reserved.
Hocus-pocus Meningococcus
From schoolyards to college campuses, masters of deception levitate in the air, infiltrate large groups of people, and finally decimate central nervous systems with sleight of hand. Bacteria, mycobacteria, fungi, spirochetes, protozoa, helminths, and viruses are their names, but on their marquees is emblazoned a simple, “MENINGITIS.” As beguiling as Houdini, they often seek instant gratification, presenting acutely to a virtually limitless audience within hours to 1-2 days after the appearance of nonspecific cold or flu symptoms. On a whim, they may prolong their tours, performing less frequently, with hiatuses of weeks to months of general symptoms. Let there be no mistake, however, what they are selling is not pure entertainment, but medical emergency.
Their youngest fans are 3 months old and lie in cribs. Their oldest lie in nursing homes, and no one inbetween is immune to their charms. With enigma as a tool of their trade, they often go undiagnosed until the final act. One-third of meningitis cases, in fact, go undetected despite careful laboratory evaluation.
In order to banish our infectious friends in a “puff of smoke,” we must first understand what we are up against. It is common knowledge that meningitis is an infection and inflammation of the membranes, which are called meninges, and cerebrospinal fluid (CSF) surrounding the brain and spinal cord. With the advent of current vaccines, there has been a shift in preferred “live targets,” from children younger than 5 years old to the 15-24-year-old age group and older adults. Audiences, too, have indeed become “captive,” with 700 Americans dying of meningitis each year.
Viral meningitis, also called aseptic meningitis, usually results from the spread of enteroviruses through direct contact with respiratory secretions (e.g., saliva, sputum, or nasal mucus) of an infected person. It causes signs and symptoms for 10 days, followed by resolution on its own. Supportive intervention is all that is needed, and the cause may never actually be found. Have you ever asked a magician where the rabbit he has pulled out of his hat comes from?
Bacterial meningitis, on the other hand, is the stuff of sorcerers, Wiccans, and wizards. It is much more serious than viral meningitis, and the curtain goes up when infection in another area of the body threads blood vessels and a path to the meninges. Signs and symptoms are varied, but, with over 50,000 hospitalizations in the U.S. each year due to some form of meningitis and its nefarious bag of tricks, it pays to be vigilant. In addition to the common manifestations of the malady listed above, others include neck stiffness, vomiting, seizures, lethargy, delirium, and focal neurologic signs, the latter particularly alarming and requiring a computed tomography (CT) scan to rule out cerebral edema.
Timely diagnosis relies on the thrust of a magic wand, commonly known as a lumbar puncture needle, between lumbar vertebrae L4 and L5 for collection of cerebrospinal fluid (CSF). Analysis of the opening pressure, color, culture, number of red and white blood cells, glucose, and proteins of that ethereal nectar is confirmatory to both the diagnosis of the disease itself and its etiologic agent.
That leaves only the esoteric pièce de résistance to put an end to the harbingers of meningitis before they put an end to us. If meningitis is not eliminated immediately, presto chango, permanent neurologic sequelae, hearing loss among others, will inevitably result. Antibiotic therapy, for a minimum of 7 days and a maximum 3-4 weeks, depending on the bacterial agent involved, is the name of the game. With a clear and proactive focus, there is no need for hocus-pocus.
Copyright 2005, Albert M. Balesh, M.D. All rights reserved.
Saturday, July 08, 2006
Terminator versus Defibrillator
Our last stand is imminent, and no prisoners will be taken in the ultimate sacrifice to our vanity and disbelief. We were warned of the “Terminator’s” coming, and, yet, we chose to live the “good life” and forget that the inevitable was already on hand.
Now, only one thing stands in the way of our immediate demise. A secret weapon! Research and development has provided us with a fully affordable system that can even the score, and reduce the commissions of real estate agents dealing in cemetery properties. The “Defibrillator” is here, and perhaps we have a chance, after all.
Heart failure, our worthy but utterly ruthless foe, represents a major public health problem in all industrialized nations. Dress a developing world’s population in the trappings and vestments of the modern world, and it, too, will find itself naked to the onslaught. Each year in the United States alone, heart failure infiltrates our unsuspecting, elderly troops, to the tune of almost 1 million hospital admissions and 50,000 deaths. Its incidence and prevalence is on the rise, and they are likely to increase still further as our population ages. So, let the “baby boomers” beware! No solace can be taken in a contemporary “Lili Marlene,” “Radio Free Europe,” or “Radio Saigon.”
The current battle plan and medical logistics are particularly important to me, as my father was a victim of the “Terminator” on March 30, 2004. As he lay in my arms at home, and I observed first hand his rapid breathing and heart rate, wheezing and gagging, pale color of his skin, and, finally, dilated pupils and respiratory and cardiac arrest, all in a matter of minutes, I knew I was in trouble. Years of medical experience vanished at that sight, and I felt totally impotent at that moment. They say that hearing and touch are the last things to go, when someone dies. As his muscles became flaccid, I jumped into action. It was a losing battle, however, as I had neither the drugs nor instrumentation for advanced life support, as my basic life support (CPR) technique was rusty, as I knew that it would take more than six minutes for the paramedics to arrive, and as I was fully aware of the fact that even if I succeeded in resuscitating my father at home, the current medical literature suggested that there was a 75% chance that he would not make it anyway. If I had only possessed an automatic external defibrillator (AED) yesterday, I might not feel so much guilt today. “Defibrillator” might not have evened the score, but it would have leveled the playing field.
Sudden cardiac arrest kills an average of 930 people every day, and, while CPR (two lung inflations for every 15 chest compressions, and a rate of 100 compressions per minute) is an essential stopgap measure until the paramedics arrive, it usually takes longer than we would hope and pray. Severe cardiac arrhythmia or arrest without CPR within the first 4 to 6 minutes has a poor outcome even if defibrillation is later successful. The “Terminator” will inevitably triumph, when life support is not instituted within the first 8 minutes of arrest or ventricular fibrillation. Once anoxic encephalopathy (brain damage from lack of oxygen, or hypoxia) sets in, the point is mute. The patient will never be the same, and the “Good Samaritan” or family member will curse both the day he or she was born and the so-called “successful” resuscitative effort.
On September 16, 2004, the U.S. Food and Drug Administration (FDA) agreed for the first time to allow consumers to purchase AEDs, like the Philips HeartStart Home Defibrillator for $1,495, online at amazon.com, for example. It does not take a lot of know-how to use a home defibrillator, but speed and easy access to it are of the essence. “Defibrillator” must act within 5 minutes of the skirmish, in order to vanquish the “Terminator.” Shocking the heart back to some semblance of normality within that limited and precise timeframe can quadruple the chances of survival. Had “Defibrillator” been available to me on March 30, 2004, I would not feel so much guilt right now. The memories of my poor father’s demise and his ghost will haunt me forever, but the brand new portable AED in the trunk of my car will stop the “Terminator” in his tracks the next time he decides to pay a friend, family member, or innocent pedestrian a visit. That will be my “shock and awe!”
Blackbird
Some statistics will put the “bird attack” in perspective and move hands closer to the alarm bell. A typical year in the U.S. brings the deaths of 30,000 to 50,000 people as a result of influenza virus infection, and global death rates are 20 to 30 times higher. The past 300 years have seen 10 pandemics of influenza A, and the now famous pandemic of 1918 and 1919 killed 50 million to 100 million souls. The number of hospitalizations each year from 1979 to 2001 related to influenza in the U.S. reached 226,000, and 325,000 patients died in the U.S. from pulmonary and circulatory causes connected to influenza from 1990 to 1999.
Now comes the bad news. The H5N1 avian influenza virus promises to eclipse those statistics if action is not taken immediately. Although to date there have been only 100 cases of human infection with the avian virus since 19974, mutation and reassortment of genetic material are likely to shift the balance and create a highly infectious “viral monster” capable of easy spread from human to human. As the matter stands now, infected wild birds shed the influenza virus in their saliva, nasal secretions, and feces. Their domesticated “kissing cousins” contract the virus directly from their wild relatives, or through contaminated surfaces, cages, water, or feed.
Hapless humans in direct or close contact with domesticated chickens, ducks, and turkeys develop symptoms of fever, cough, sore throat, muscle aches, eye infections, severe respiratory illnesses (acute respiratory distress syndrome), and other life-threatening conditions. To halt the onslaught, killing the birds, the chicken farmers, and their progeny might have been a suitable solution for Pharaoh, but civilized man is a humane creature. His arsenal is a ban on poultry importation, a limitation of travel, and prescription medicines, some of which have already been rendered impotent by viral resistance. Stop-gap measures simply cannot win the day.
Questions continue to abound, and expedited solutions are not forthcoming. Mechanical ventilators are in short supply, and it will take a while for cell-culture technology for production of vaccine to replace the current egg-based manufacturing process. Furthermore, most vaccines are manufactured abroad. The U.S. might have contemplated a similar “doomsday scenario” when it decided to become a service economy, close down factories, and export manufacturing plants overseas and to countries where the per capita income is pennies to the dollar.
Ramping up vaccine production would require a minimum of six months, and that only after isolation of the circulating strain of virus. Supplies of those vaccines during those months might reach doses sufficient to vaccinate perhaps 500 million people, or roughly 14% of the world’s population.1 Perhaps Pharaoh’s idea would not be so bad in the long run, after all. The extremely limited supply of antiviral agents and vaccine might even mandate it.
Enough bickering. Is it too late? What are the options? Where do we go from here? U.S. health authorities must “come clean,” and develop a system of risk communication in order to allay the public’s fears. A detailed plan for vaccine and antiviral agent allocation and stockpile positioning will also be needed, and unpopular decisions are going to have to be made in the short-term, in order to prevent devastation in the long-term. Vaccination of health care workers at the expense of our children might be one such unfavorable stance to take. After all, sick doctors and nurses would put us all in jeopardy.
If cell culture-based technologies for vaccine production are not developed, implemented, and sustained in short order, we may become the birds on holiday tables.
Copyright 2005, Albert M. Balesh, M.D. All rights reserved.
Fall from Grace
Young and old, rich and poor, no one is immune. Underdeveloped countries, with their utter lack of adequate medical services, stagnant economies, and nonexistent patient education have borne the brunt of the attack. This becomes even more obvious when we consider that 85% of the deaths related to this malady in 2004 occurred in women who had never been screened via Pap smear. When an ounce of prevention is truly a matter of life and death, and when cures can be instituted only at the sound of early alarms, every effort must be made to follow the recommendations of the American Cancer Society and the American College of Obstetrics and Gynecology. While the former strongly suggests two consecutive yearly Pap smears in women after onset of sexual activity, or older than age 20, with repeat every 3 years, the latter recommends yearly Pap smears with routine annual pelvic and breast examination.1 Life is oftentimes unfair, and, while the U.S.-based protocols are fine and dandy for our own citizens, what about those less fortunate?
Cervical cancer is the major gynecologic cancer in the Third World, where poverty, early initial sexual activity, multiple partners, and smoking contribute to its prevalence. In both the U.S. and internationally, its cause has been linked to sexual transmission of the human papilloma virus (HPV). Currently, promising studies are underway to create a low-cost vaccination to HPV and subsequent solution to the problem of provision of affordable preventive measures to underdeveloped areas of the world. Screening via repeat Pap smears (90-95% accurate in detecting early lesions of cervical cancer) and follow-up are simply not feasible in those regions. Screening strategies involving a two-visit, visual inspection of the cervix by a healthcare professional and viral DNA testing are being examined as possible, cost-effective alternatives to traditional, three-visit screening programs employing Pap smear in this country.2 After all, right to life is God-given, and must not be subservient to national origin, race, or simply luck of the draw.
Regardless of which side of the tracks, fence, or border a woman is born on, the signs of cervical cancer are unmistakable, and should at the least incite “healthy suspicion” and immediate visit to a qualified healthcare professional. While procrastination is human and no one likes to be pinched and prodded, failure to recognize the signs of abnormal bleeding and postcoital spotting, intermenstrual or prominent menstrual bleeding, yellowish vaginal discharge, low back pain, and urinary symptoms can be downright fatal in the long run. Immediate action is called for in those cases. It goes without saying that the earlier the diagnosis and treatment of cervical cancer, the greater the chances of success and the longer the survival rate.
Depending on the stage of the disease, treatment modalities run the gamut from biopsy and abdominal hysterectomy to radiation therapy and chemotherapy. Combinations of these elements are no more effective than the single regimens themselves, and advanced stage cervical cancer has a five-year survival rate of only 7%. Why, oh why, did those women (and their partners) not take prevention more seriously?
While it was too late for my friend, if this short piece in an obscure quotidian crosses the desk and catalyzes preventive gynecologic examination of just one reader, then her “fall from grace” will serve as a fitting epitaph and message of salvation.
Young and old, rich and poor, no one is immune. Underdeveloped countries, with their utter lack of adequate medical services, stagnant economies, and nonexistent patient education have borne the brunt of the attack. This becomes even more obvious when we consider that 85% of the deaths related to this malady in 2004 occurred in women who had never been screened via Pap smear. When an ounce of prevention is truly a matter of life and death, and when cures can be instituted only at the sound of early alarms, every effort must be made to follow the recommendations of the American Cancer Society and the American College of Obstetrics and Gynecology. While the former strongly suggests two consecutive yearly Pap smears in women after onset of sexual activity, or older than age 20, with repeat every 3 years, the latter recommends yearly Pap smears with routine annual pelvic and breast examination.1 Life is oftentimes unfair, and, while the U.S.-based protocols are fine and dandy for our own citizens, what about those less fortunate?
Cervical cancer is the major gynecologic cancer in the Third World, where poverty, early initial sexual activity, multiple partners, and smoking contribute to its prevalence. In both the U.S. and internationally, its cause has been linked to sexual transmission of the human papilloma virus (HPV). Currently, promising studies are underway to create a low-cost vaccination to HPV and subsequent solution to the problem of provision of affordable preventive measures to underdeveloped areas of the world. Screening via repeat Pap smears (90-95% accurate in detecting early lesions of cervical cancer) and follow-up are simply not feasible in those regions. Screening strategies involving a two-visit, visual inspection of the cervix by a healthcare professional and viral DNA testing are being examined as possible, cost-effective alternatives to traditional, three-visit screening programs employing Pap smear in this country.2 After all, right to life is God-given, and must not be subservient to national origin, race, or simply luck of the draw.
Regardless of which side of the tracks, fence, or border a woman is born on, the signs of cervical cancer are unmistakable, and should at the least incite “healthy suspicion” and immediate visit to a qualified healthcare professional. While procrastination is human and no one likes to be pinched and prodded, failure to recognize the signs of abnormal bleeding and postcoital spotting, intermenstrual or prominent menstrual bleeding, yellowish vaginal discharge, low back pain, and urinary symptoms can be downright fatal in the long run. Immediate action is called for in those cases. It goes without saying that the earlier the diagnosis and treatment of cervical cancer, the greater the chances of success and the longer the survival rate.
Depending on the stage of the disease, treatment modalities run the gamut from biopsy and abdominal hysterectomy to radiation therapy and chemotherapy. Combinations of these elements are no more effective than the single regimens themselves, and advanced stage cervical cancer has a five-year survival rate of only 7%. Why, oh why, did those women (and their partners) not take prevention more seriously?
While it was too late for my friend, if this short piece in an obscure quotidian crosses the desk and catalyzes preventive gynecologic examination of just one reader, then her “fall from grace” will serve as a fitting epitaph and message of salvation.